Transforming insurance reimbursement into a digital experience
Pacifico Insurance Company
Digital transformation | UX/UI | Service design
Team
Full time: 1 product owner, 1 innovation analyst, 2 UX/UI designers, 1 design intern, 1 frontend developers, 1 backend developer, 1 innovation architect.
Part time: 1 scrum master, 1 QA, 1 IT analyst.
Role
Designed the web app for users to claim reimbursements and the back-office for employees to develop tasks.
Conducted interviews and shadowed actual and potential reimbursement users, stakeholders, and other service participants.
Prototyped and conducted user testing for both the web app and back-office website.
Shared new work methodologies with the team and coached them in research methods.
Co-created workshops and release meetings and spoke at intern events about our project.
As I am passionate about video making and storytelling, I created photos and videos for the lab, including tutorial videos, stakeholder interviews, and other internal videos.
Summary
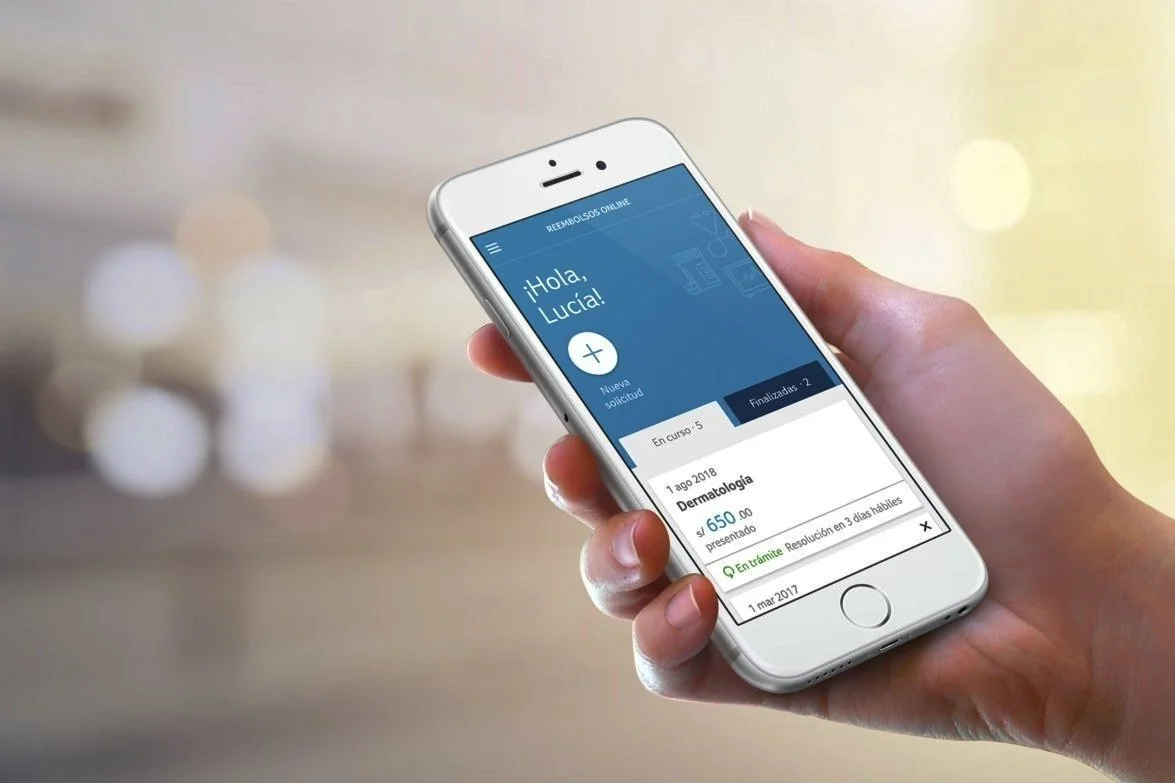
Web app designed so our health clients can claim reimbursements online in a more accessible way by sending pictures of their expenses after visiting the doctor.
This new process allows users to make a claim whenever and wherever they want without commuting to Pacifico's office.
This project was the first one commissioned to the innovation lab to lead Pacifico's digital transformation and start improving the experience clients have with Pacifico's services.
Click play in the video to see a summary of this project.
Context
About health reimbursement claims in Pacifico
The satisfaction rate for health reimbursement services in Pacifico was among the lowest. As a result, the innovation lab was commissioned with its first project to improve user satisfaction and restore the company's relationship with its clients.
The project's primary goal was to enhance the experience of health insurance clients who received reimbursement. These clients were among the top ones who paid for the most expensive products but required better services and experiences. Moreover, these users had high purchasing power and could afford to purchase other products from the company if they had a good experience.
Objective
Improve user satisfaction to restore Pacifico's relationship with its most valuable clients.
Process
My team was assigned this project because it required the application of design thinking and agile methodologies. It was a multidisciplinary project that brought together designers, developers, and business analysts at Pacifico to work towards a common goal.
At the start of the project, the team received coaching from Designit, a design consultancy firm that was the strategic partner of the innovation labs responsible for assessing design methodologies.
Comprehension, ideation and definition
Research and kick-off workshop
We interviewed users, brokers, stakeholders, and back-office actors. We also spoke with heavy users to understand their pain points and experience with the process. We used shadowing for brokers and back-office actors and interviewed stakeholders. Then, we held a workshop to align everyone's vision and co-create an ideal solution based on our findings.
Concept workshop
At the workshop, we presented the project timeline, prioritized solution components, and wireframes for the web app. We explained the scrum methodology for working in sprints and exhibited a blueprint (A) to help understand the complex service with many actors.
Working in sprints
Throughout the project, I designed the web app (B) for clients and the back-office web (C) for doctors, assistants, executives, and payment employees. I iterated the designs with users and back-office actors until the final launch.
A. Service Blueprint
B. Web App Screens
B. Back Office Web Screens
Launch
Launching and transferring the web app
The team developed and launched a new web app for our three main health insurance plans within a year. The project was the first to be created in our innovation lab, and we supported it for a while, aiming for an 80% customer satisfaction rate before handing it over to another team. However, it exceeded our goal and achieved an 87% customer satisfaction rate in only five months, so we assigned it to the health and technology team.
This experience taught us a lot, and we planned to incorporate the web app into a more extensive platform in the future that would allow users to manage all their insurance products.